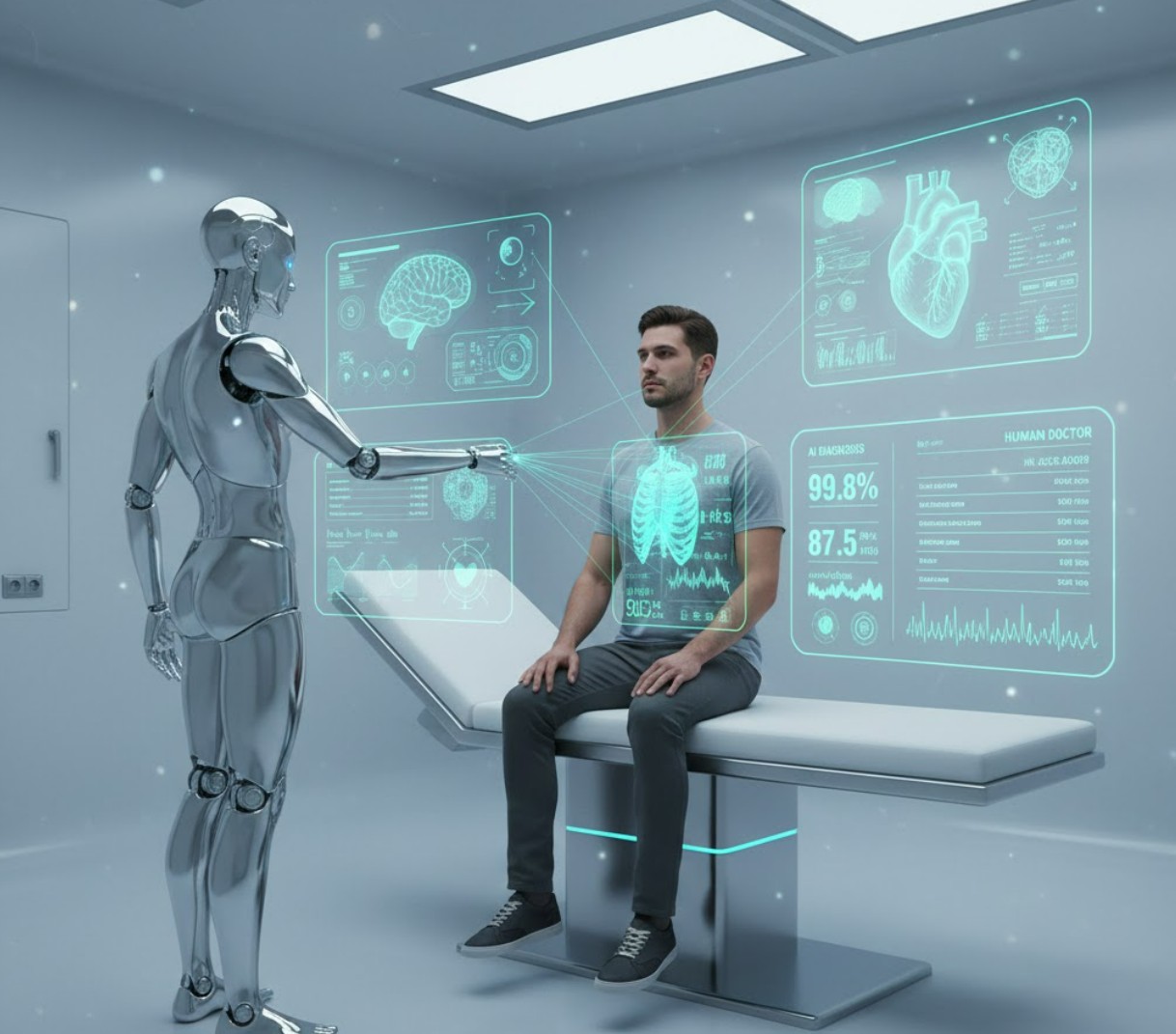
The integration of Artificial Intelligence (AI) into healthcare is rapidly transforming the landscape of medicine, promising a future where health checkups are faster, more accessible, and potentially more accurate.
From sophisticated diagnostic algorithms analyzing medical images to virtual assistants fielding initial patient symptoms, AI is moving into the consultation room. This raises a fundamental and compelling question: In the era of virtual care, are AI-powered doctors surpassing human clinicians in diagnostic accuracy?
The AI Advantage: Speed, Scale, and Pattern Recognition
AI’s strength lies in its ability to process and analyze vast amounts of data at speeds and scales unattainable by human physicians. Machine learning and deep learning models are trained on millions of medical records, images, and clinical case studies, allowing them to identify complex patterns and subtle indicators of disease that may escape the human eye.
Superior Image Analysis
One of the clearest areas where AI demonstrates superior performance is in the analysis of medical images. Studies in specialties like radiology and ophthalmology have shown AI systems achieving diagnostic accuracy comparable to, and in some cases, exceeding, human experts.
-
Radiology: AI algorithms trained on mammograms or chest X-rays have demonstrated an ability to detect early signs of cancer or other diseases with remarkable precision. A landmark Swedish trial found an AI-assisted approach in mammography screening identified 20% more breast cancers while significantly reducing the radiologist workload.
-
Ophthalmology: AI models can detect diseases like diabetic retinopathy from retinal scans with accuracy on par with highly experienced ophthalmologists.
-
Pathology: AI excels at analyzing tissue samples, helping to classify and grade tumors faster and more consistently than human pathologists.
This enhanced capability is due to AI’s consistency and lack of fatigue—it can maintain peak diagnostic performance through thousands of scans, day or night, a factor that invariably impacts human performance.
Adherence to Clinical Guidelines
Another key advantage highlighted in recent research is AI’s strict adherence to established medical guidelines. A study comparing AI recommendations with those of physicians in a virtual urgent care setting found that the AI’s diagnostic and treatment suggestions were rated as optimal more often and were less frequently considered potentially harmful. The AI consistently applied guidelines, such as avoiding unnecessary antibiotic prescriptions for viral infections, demonstrating a level of systematic, evidence-based practice that human clinicians, subject to human factors like memory and bias, can sometimes miss.
The Human Edge: Clinical Reasoning and Context
Despite AI’s power in pattern recognition, the human physician retains a crucial, irreplaceable role, primarily rooted in clinical reasoning, contextual understanding, and the intangible element of human connection.
Nuanced Clinical Reasoning
Clinical reasoning involves more than just recalling facts or identifying a pattern; it requires the ability to integrate new, uncertain, or even irrelevant information, prioritize symptoms, and dynamically adjust a diagnostic path. This is an area where advanced AI, particularly large language models (LLMs), still struggles.
-
Adapting to Uncertainty: When faced with changing clinical information—or “red herrings”—human doctors are better at discerning what truly matters and pivoting their diagnostic “scripts.” LLMs, in contrast, sometimes struggle to update their judgment in response to new, nuanced, or conflicting patient data, leading to potentially convincing, yet incorrect, diagnoses.
-
Holistic Assessment: A human doctor assesses a patient holistically. They interpret non-verbal cues, gauge a patient’s level of distress, understand the psychosocial context, and factor in a patient’s complete history in a way that structured AI inputs cannot fully capture. For instance, a doctor can observe a COVID-19 patient’s subtle breathing pattern and correctly assess a reported “shortness of breath” as mild congestion, whereas an AI, relying only on the reported text, might trigger an unnecessary emergency referral.
The Value of Human Interaction
Medicine is not just a technical exercise; it’s a relational profession. The patient-physician relationship is built on trust, empathy, and effective communication.
-
-
Empathy and Trust: While some AI chatbots have been found to generate responses that are perceived as more empathetic than some clinicians in text-based studies, patients still overwhelmingly express greater trust in a diagnosis delivered by a human physician. This “algorithm aversion” suggests that for high-stakes decisions like medical diagnosis, the human element provides a necessary sense of accountability and psychological comfort.
-
Information Gathering: A skilled doctor knows how to guide a conversation, ask the right follow-up questions, and elicit crucial details that a patient may not know are important. Studies have shown that when AI systems attempt to conduct a direct patient interview, their diagnostic accuracy can plummet, underscoring the vital role of the human in the initial data-gathering phase.
-
The Future is Collaborative: AI as a Co-Pilot
The prevailing consensus among experts is that the future of diagnostics is collaborative, not competitive. The goal is not to replace the doctor but to create a powerful human-AI partnership where each compensates for the other’s limitations.
The Optimal Partnership Model
The most effective models leverage AI’s strengths for screening, triage, and data analysis, reserving the human clinician for complex cases, contextual judgment, and treatment implementation.
-
Initial Screening and Triage: AI can handle the initial screening of routine cases (e.g., classifying a normal medical image) or prioritize urgent cases in the emergency room, freeing up physician time.
-
Augmented Decision-Making: AI acts as a “second opinion” or an alert system, bringing subtle patterns or risks to the doctor’s attention. The physician, armed with this AI-driven insight, then applies their clinical judgment and contextual understanding to finalize the diagnosis and treatment plan. This synergistic model can potentially reduce diagnostic errors caused by human bias or oversight.
-
Personalized Medicine: AI’s ability to analyze genomic data, patient history, and real-time monitoring from wearable tech allows for the development of truly personalized treatment plans, predicting patient responses to medication and optimizing dosages with unprecedented precision.
Challenges in Implementation
For this collaborative future to be realized, several significant challenges must be addressed:
-
-
Data Bias and Ethics: If AI models are trained on datasets that do not adequately represent all demographics, they can perpetuate and even amplify existing health disparities and algorithmic bias, leading to inaccurate diagnoses for certain patient groups.
-
Regulation and Liability: Clear legal and regulatory frameworks are needed to determine accountability when an AI system makes a diagnostic error.
-
Clinician Training: Doctors require formal training on how to effectively integrate and interpret AI’s input without becoming overly reliant on the technology or under-valuing their own expertise.
-
Conclusion
Are AI-powered health checkups more accurate than humans? The nuanced answer is: It depends on the task. For high-volume, pattern-recognition tasks like image analysis, AI can equal or surpass human performance in terms of speed and consistency. However, for the intricate process of clinical reasoning and the holistic, empathetic care required in a full patient consultation, the human doctor remains the indispensable expert.
The most exciting progress lies in combining the analytical power of the machine with the compassionate judgment of the physician. The virtual doctor is not a replacement but a powerful co-pilot—a tool set to make the human doctor faster, more accurate, and ultimately, able to deliver a higher quality of care to a greater number of people.